What Causes A Migraine:
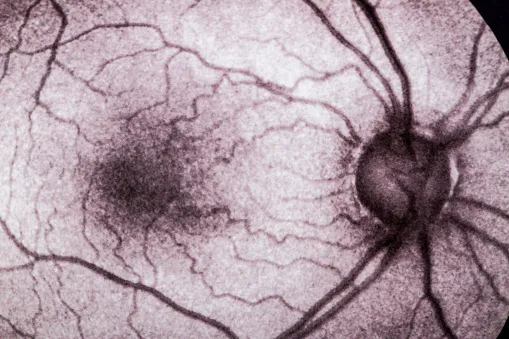
The most common cause of recurring, disabling headache pain, migraines are also the most common underlying cause of disabling chronic, daily headache pain. While migraines are the No. 1 reason that patients see a neurologist, most cases are handled by primary care physicians. In up to 25 percent of patients, the migraine headache pain may be preceded by an aura, a temporary neurological syndrome that slowly progresses and then typically resolves just as the pain begins.
The interprofessional care provided to the patient must use an integrated care pathway combined with an evidence-based approach to planning and evaluating all joint activities. Primary care clinicians (MDs, DOs, NPs, and PAs) obtain the assistance of an internist, a neurologist, or a headache specialist if there’s any doubt about the diagnosis. Nurses and psychologists can assist team management by teaching lifestyle changes, mental health supervision, drug overuse detoxification, and medication use recommendations. Most people with migraine will have spontaneous attacks, meaning there is nothing they did or didn’t do to trigger the attack. Some people will have attacks that have an identifiable cause. Everyone has different triggers, but there are a few common culprits that affect a large number of people.
There also may be a pain sensitization phenomenon at work. Simply put, with long-lasting pain, a person’s nervous system stays in a chronically activated state, lowering their threshold for experiencing pain and making them hypersensitive to pain. Preventive treatments are designed to reduce the frequency, severity, and duration of attacks of migrainebefore they occur. These treatment options can be medical, such as medications or procedures, and non-medical, such as devices, lifestyle changes, trigger avoidance, behavioral therapy, or physical therapy. There are 2 types of medicines for migraine treatments (abortive and preventive). One type, called ‘abortive,’ focuses on stopping the headache from becoming severe and relieving the headache pain.
The US headache consortium has given relaxation therapy, cognitive behavioral therapy, and biofeedback Grade A evidence for migraine prevention [77]. Most, if not all, of these behavioral treatments include improvements in stress management as well as adjusting expectations and perceptions as therapeutic targets. However, in many of the studies of behavioral interventions, it has been illustrated that the reduction in headache frequency is not a function of the intended beneficial target organ response [51, 78,79,80].
While it is doctor-verified, it is not intended to serve as medical advice, and users are advised to seek the advice of their doctors before making any decisions based on the information in this article. Reviewed for accuracy by the American Migraine Foundation’s subject matter experts, headache specialists and medical advisers with deep knowledge and training in headache medicine. Children who have abdominal migraine are likely to develop more typical migraine symptoms as adults.
People of Color are less likely to receive the diagnosis of migraine and the treatment than white people. Genetic features may also play a role ‘ having a family history of see migraine is a common risk factor. At this stage, a person might experience a ‘prodrome,’ which may involve emotional changes, specifically depression and irritability.
Still, we are likely far from the plausible biological roof for forecasting migraine attacks. Because there is such a wide spectrum of disease severity with migraine, there’s also a wide spectrum of management plans. Some people need what we call an acute or a rescue treatment for infrequent migraine attacks. Whereas other people need both an acute and a preventive treatment plan. Preventive treatment reduces the frequency and severity of migraine attacks.
If you have migraines and take medications for them more than 10 days in a month, you may be setting yourself up for what’s called a rebound headache. Your doctor will probably call it a medication overuse headache. Be careful when you take OTC pain meds because they might also add to a headache. If you use them too much, you can get rebound headaches or become dependent on them.
There are also a number of non-medical treatments designed to help minimize migraine pain and frequency. One is an electrical stimulation device, which has been approved by the FDA. It is a headband that you wear once a day for 20 minutes to stimulate the nerve linked to migraines. Another non-medical treatment is counseling aimed at helping you feel in more control of your migraines.
For more of the latest news and information on migraine, visit the AMF Resource Library. For help finding a healthcare provider, check out our Find a Doctor tool. Acute treatments are taken when you are experiencing an attack and are designed to stop it before it gets worse. These include over-the-counter pain relievers, prescription medications, or devices that stop the pain.
For example, there is another protein that’s called PACAP that’s under investigation. And we will continue to identify additional molecules and proteins until we find treatment options for every single person with migraine. page These are all FDA approved for the as-needed treatment of migraine, and some are also approved for preventive treatment. Another new as-needed medication that’s not CGRP-related is called lasmiditan (Reyvow).
However, a combination of genetics and environmental triggers is a possible cause. Migraine pain likely occurs due to functional and structural changes in the brain and environmental triggers. the advantage The information on this site should not be used as a substitute for professional medical care or advice. Contact a health care provider if you have questions about your health.
Over-the-counter migraine medications are effective if you have mild to moderate migraine symptoms. The main ingredients in pain-relieving medications are ibuprofen, aspirin, acetaminophen, naproxen and caffeine. When you have a headache, specific nerves in your blood vessels send pain signals to your brain.