Ibs And Anxiety:
For example, some selective serotonin reuptake inhibitors (SSRIs) commonly prescribed for panic disorder have also been found to reduce IBS symptoms. On the other hand, some of the medications for panic disorder can worsen IBS symptoms, so it is important that you discuss your symptoms and treatment options with your doctor. First, given the overlap between anxiety and depression, it could be that the increased risk is due to general psychological distress ‘ and not specifically anxiety or depression. In other words, simply being more stressed could increase your chances of developing IBS. Second, given that the studies involved were correlational, it’s unclear whether this stress directly influences the development of IBS or whether it does so through other means. For instance, it could be that individuals chronically high in stress are more likely to eat foods that can irritate the lining of the gastrointestinal tract, leading to the development of IBS.
“Living with IBS is about more than just managing symptoms, it’s about reclaiming control over your life. It’s about understanding that every challenge we face is an opportunity to learn more about our bodies and how to care for them Click here to read more...”
Just keep in mind that there are known side effects with tricyclics like difficulty sleeping and urinating, dizziness, sexual challenges, and a dry mouth. check these guys out share some common causes and triggers that are related to the gut-brain axis and biopsychosocial model as discussed above. Walking, running, swimming, and other physical activities can reduce stress and depression.
They also noted that increasing abdominal symptom severity often correlated with increasing severity of anxiety symptoms. Other evidence suggests that the two conditions often occur together and may worsen each other’s symptoms. IBS symptoms may improve through PTSD treatment if PTSD is exacerbating your symptoms.
“The journey to managing IBS begins with a single step. It’s about embracing the power of dietary changes, stress management, and medical treatments. Remember, health is wealth, and your well-being is worth every effort Click here to read more...”
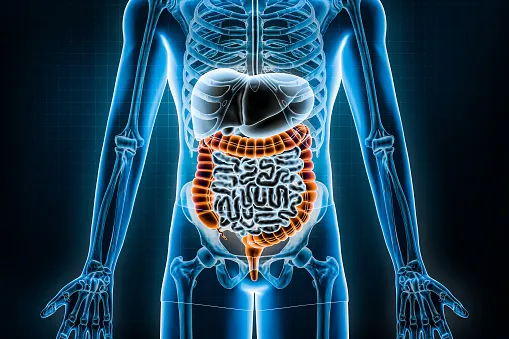
People with agoraphobia display many avoidance behaviors in which they steer clear of places and situations that they fear will trigger panic attacks or that escape might be difficult or embarrassing. Although IBS is not a life-threatening illness, it often develops into a chronic condition that can greatly impact many aspects of one’s life. This is especially problematic for people with IBS because their brains are more responsive to pain signals from the GI tract, so they tend to perceive pain more acutely than others, according to Harvard Health Publishing.
Thus, for their investigation, the researchers used an approach known as a meta-analysis. Whereas a typical study may examine only 100 participants, meta-analyses combine data from upwards of hundreds of studies, sometimes including source thousands of individual participants, into a single analysis. This approach allows researchers to take into account differences across a number of studies, helping them to understand the nuances of a particular effect.
“Managing IBS isn’t just about treating symptoms, it’s about addressing the root cause. It’s about building a lifestyle that promotes gut health and overall well-being. Remember, a healthy gut is the key to a healthy life Click here to read more...”
Because no direct cause-and-effect link between PTSD and IBS has been established, it’s possible to experience these conditions simultaneously (comorbidly) but with symptoms occurring independently of one another. The connection of your gut-brain axis is why you might experience an upset stomach when you’re upset, for example, or why certain foods can affect your mood. PTSD doesn’t always cause GI distress, but, when it does, your gut-brain axis and natural stress response might have something to do with it. Laura says she was “fobbed off” by some healthcare professionals who, she says, dismissed her condition and recommended laxatives for one of her symptoms – constipation. Fatigue and anxiety have significant effects on your mental health and influence actions related to your physical well-being… If you or someone you know thinks you are suffering from anxiety then take this quick online test or click to learn more about the condition.
CBT can also help you develop new coping skills and relaxation techniques. When your brain perceives a stressor, it kicks off a multitude of physiological responses to help you overcome the present challenge. Speak to your GP if you have ongoing feelings of low mood, stress or anxiety that are affecting your daily life or impacting your ability to manage your IBS. Laura Tebbs, who is 34 and from Cambridge, has experience living with IBS symptoms and anxiety and depression.
“Embrace the journey of managing IBS. It’s about understanding that the road to health is often paved with challenges. But remember, it’s these challenges that shape us, that make us stronger, that make us healthier Click here to read more...”
University training has been properly documented, as a time of anxiety, depression and high stress, especially in the examination period. A study on students analyzed the relationships between the presence of irritable bowel syndrome (IBS) and generalized anxiety disorder (GAD), chronic worry, neuroticism, anxiety sensitivity and anxiety about visceral sensations. The data was obtained using the Penn State Worry Questionnaire (PSWQ), the Neuroticism subscale of the Eysenck Personality Questionnaire, the Anxiety Sensitivity Index (ASI) and five additional items designed to measure visceral anxiety. IBS was correlated with a higher frequency of anxiety, GAD and greater worry, neuroticism and visceral anxiety. Moreover, logistic regression analyses showed that the measure of anxiety specific to visceral sensations was the strongest predictor of IBS diagnostic [7].
The present review identified articles, most of them prospective clinical studies, on the relation between anxiety and IBS during natural evolution or after therapy. The conclusion was that approximately half of IBS patients reported anxiety and/or depression and the IBS-D patients with history of psychiatric symptoms reached the disease in early ages. Other frequent complaints were linked with poor appetite, thoughts of death or dying, trouble falling asleep, disturbed sleep, and feelings of guilt. These data recommend that detection and treatment of psychiatric disorders related to IBS is essential.
Then stress can make that existing pain seem even worse, Dr. Ivanina says. Researchers still need to explore this in humans to provide conclusive evidence that the effects are consistent with animal studies. Sam Hunley holds a doctorate in cognitive psychology from Emory University. He pursued his Bachelor’s degree in psychology from Furman University and a master’s from Emory. Sam’s research, alongside Dr. Stella Lourenco, focuses on human perception of the space surrounding the body, exploring the impact of anxiety and phobias on this perception.
Similarly, do not ask for personal information from other participants. Any comments that ask for telephone, address, e-mail, surveys and research studies will not be approved for posting. “That can be helpful for urgency and for calming the system to help with diarrhea,” Riehl says. Several studies have confirmed the effectiveness of CBT in treating blog IBS, according to a July 2017 review article in the journal Psychology Research and Behavior Management. Hypnotherapy is the most common mind-body intervention used for IBS, according to the National Center for Complementary and Integrative Health (NCCIH). IBS doesn’t cause changes in bowel tissue or increase your risk of colorectal cancer.